Contraception & Unintended Pregnancy
Contraception & Unintended
Pregnancy
The Office of Population Affairs (OPA) has published guidance on steps to quality counseling.1
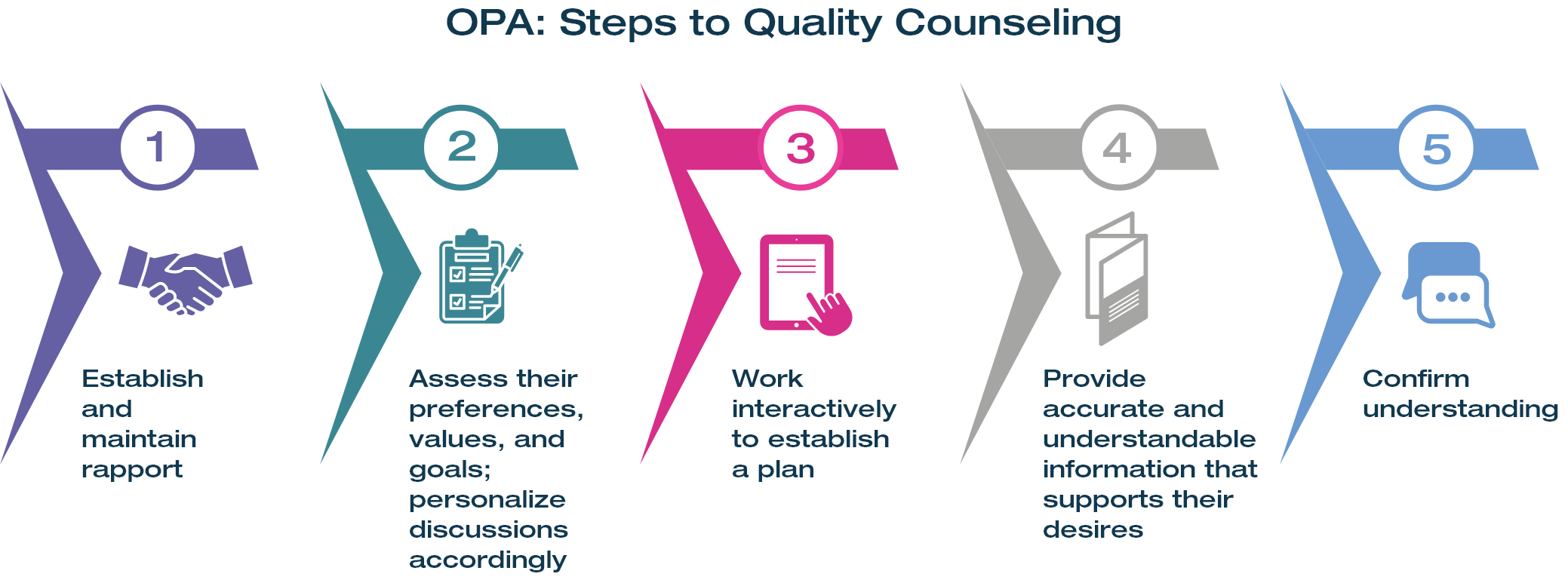
- Use simple acts such as a warm welcome, a handshake, and “taking the time to connect as human beings”
- Ensure privacy and confidentiality
- Ask permission to discuss sexual reproductive health (SRH) topics as well as inquiring, acknowledging, and centering their goals and desires for the visit
- Match the person’s tone, paraphrasing what they say, and asking if you got it right
- “What I am hearing is that you prefer……, do I have that right?”
- Focus more attention on respectful listening versus talking at them
- Open-ended questions and structured questionnaires can contribute to understanding preferences, values, and goals
- Assess the type of care and information a person might want or need and how the person prefers to receive information and make decisions
- Meet people where they are
- Avoid attempts to redirect their goals
- Set aside personal biases that may conflict with one’s preferences and work to support their desired outcomes
Example open-ended, person-centered questions to assess preferences:
- Can you tell me something (or some things) that are important to you in your contraception?
- What else are you looking for?
- Is there anything else you’re hoping to get out of your contraception?
- Is there anything you don’t want (or want to avoid) in a method?
- Providers should offer information about, and access to, a full range of hormonal and nonhormonal contraceptive options, but not prioritize one method over the other
- Establish a plan by: (1) Setting goals; (2) Using a strengths-based approach to discussing possible difficulties; and (3) Developing action plans to deal with these difficulties
- Ground all plans in their own goals, interests, and readiness for change
- Provide information that is balanced, nonjudgmental, and supported by scientific research
- Educational materials and decision aids should be offered in a variety of formats (written, audio/visual, video, interactive) to enable people to select the format that works best for them
- Consider health literacy and test all educational materials with the intended audiences for clarity and comprehension before wide-scale use, involving individuals who are representative of the populations served
- Agency for Healthcare Research and Quality (AHRQ)2 has resources to ensure materials are easy to read and understand
- Ask them to repeat back what they heard (teach-back) to confirm understanding and determine what additional information sharing may be needed2
- “I’ve shared a lot of information and I want to be sure I was clear, can you tell me what you understood about [topic]?”
References:
1. Romer SE, et al. Am J Prev Med. 2024;67(6S):S41-S86. doi: 10.1016/j.amepre.2024.09.007.
2. Health Literacy Universal Practices Toolkit, 3rd Edition. Use the teach-back method: tool 5. Agency for Healthcare Research and Quality; 2024.https://www.ahrq.gov/health-literacy/improve/precautions/tool5.html.
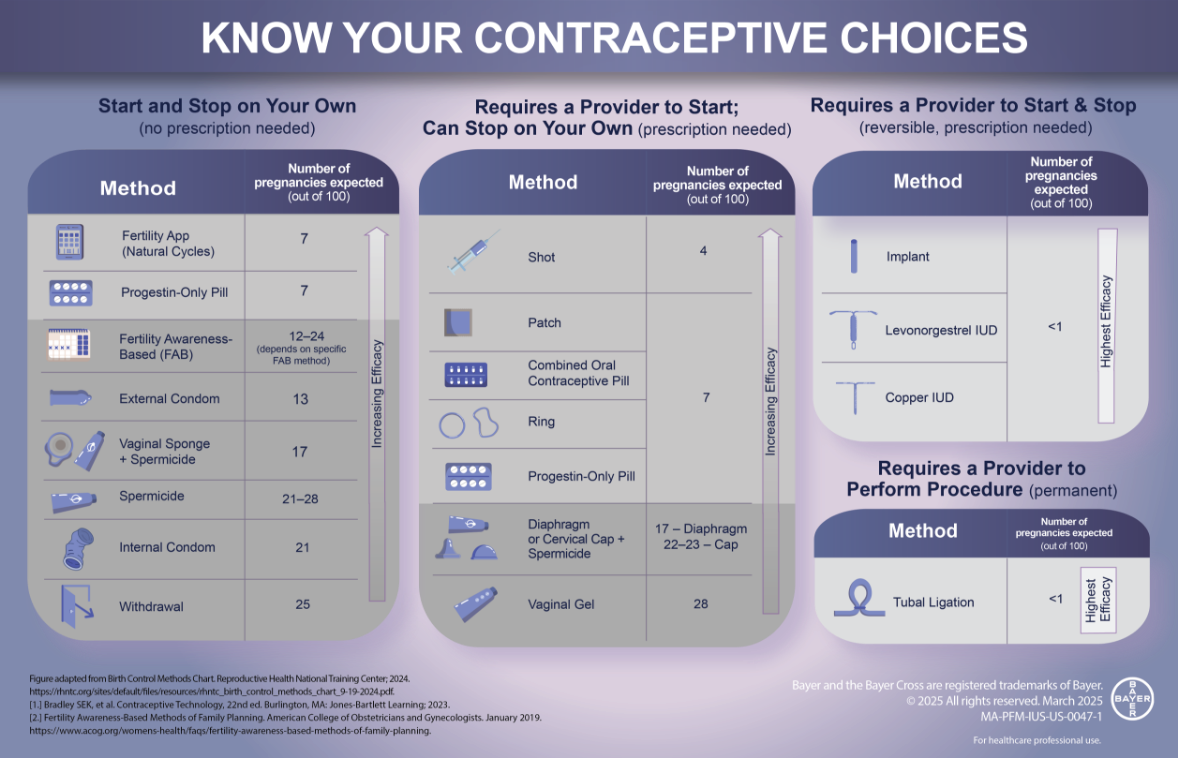
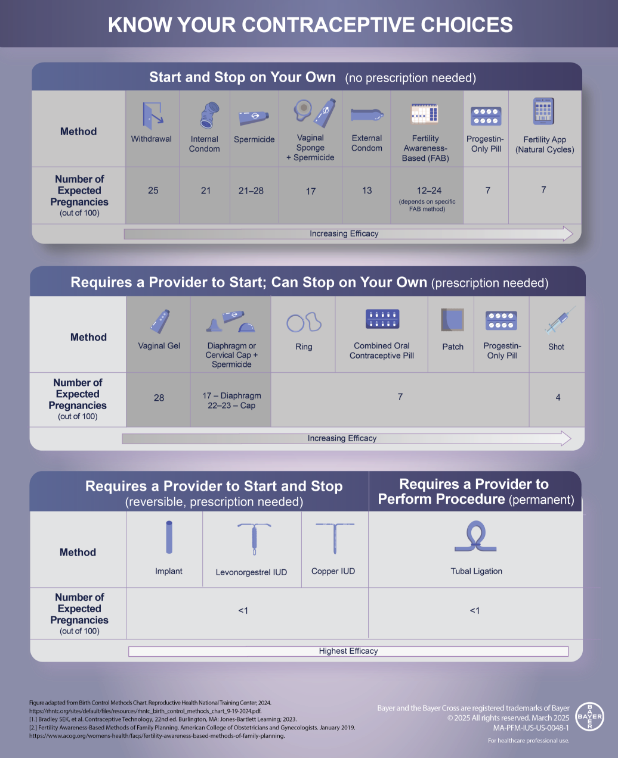
The infographic is designed to help patients consider their birth control options. The chart considers a patient’s autonomy and presents methods that they can start and stop on their own and those that require provider involvement (prescription or procedure).
Access an infographic summary (horizontal or vertical view) of the various contraceptive choices available by clicking below.
Figure adapted from: Birth Control Methods Chart. Reproductive Health National Training Center; 2024.
https://rhntc.org/sites/default/files/resources/rhntc_birth_control_methods_chart_9-19-2024.pdf.
References:
1. Bradley SEK, et al. Effectiveness, safety, and comparative side effects. In: Carson P, et al [eds]. Contraceptive Technology, 22nd ed. Burlington, MA: Jones-Bartlett Learning; 2023.
2. Fertility Awareness-Based Methods of Family Planning. American College of Obstetricians and Gynecologists; 2019.
https://www.acog.org/womens-health/faqs/fertility-awareness-based-methods-of-family-planning.
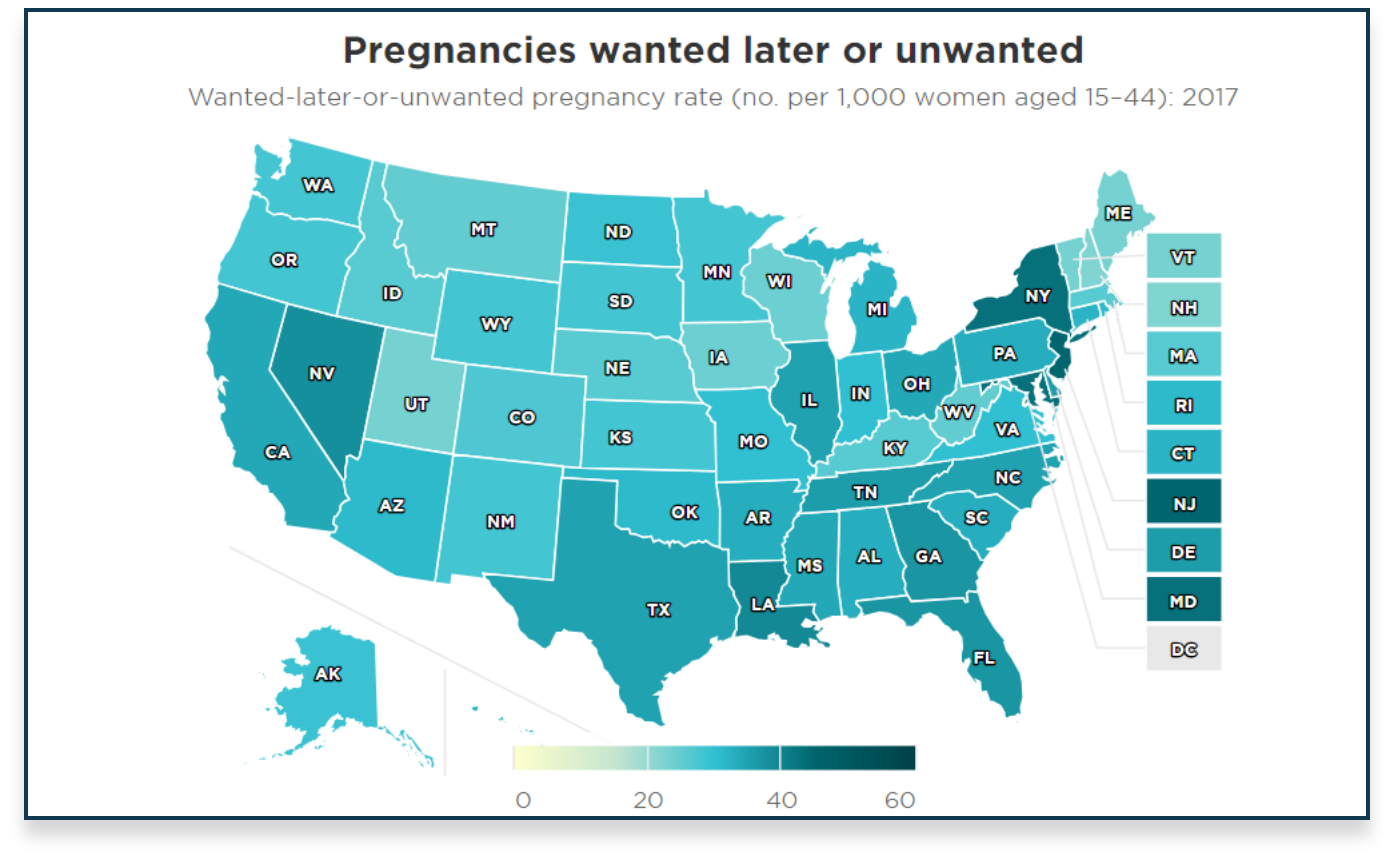
Explore this interactive resource developed by the Guttmacher Institute to find information about unintended or mistimed pregnancy in your state.
Reference:
1. Kost K, et al. Pregnancies and Pregnancy Desires at the State Level: Estimates for 2017 and Trends Since 2012. Guttmacher Institute; 2021. https://www.guttmacher.org/report/pregnancy-desires-and-pregnancies-state-level-estimates-2017.
Watch the videos below to learn more about patient-centered contraceptive counseling, using open ended questions to initiate contraceptive discussions and insights into addressing misinformation.
Explore All Videos
Contraceptive Counseling: Anita Nelson, MD
Part 1: Addressing Misinformation In the first part of the video, Dr. Anita Nelson discusses how she approaches contraceptive counseling in the age of social media and misinformation. She offers insight on how to address misinformation while offering accurate and balanced information that allows patients to make informed choices about their birth control.
Part 2: Efficient Counseling QuestionsIn the second part of this video, Dr. Anita Nelson discusses an approach to open the conversation about contraception, using a short question, “How do you think you’d feel if you got pregnant in the next year?”
Patient Centered Counseling: Anita Nelson, MD
Dr. Anita Nelson gives her perspective about the importance of patient centered counseling, listening to patients, and giving them ample opportunity to ask questions.
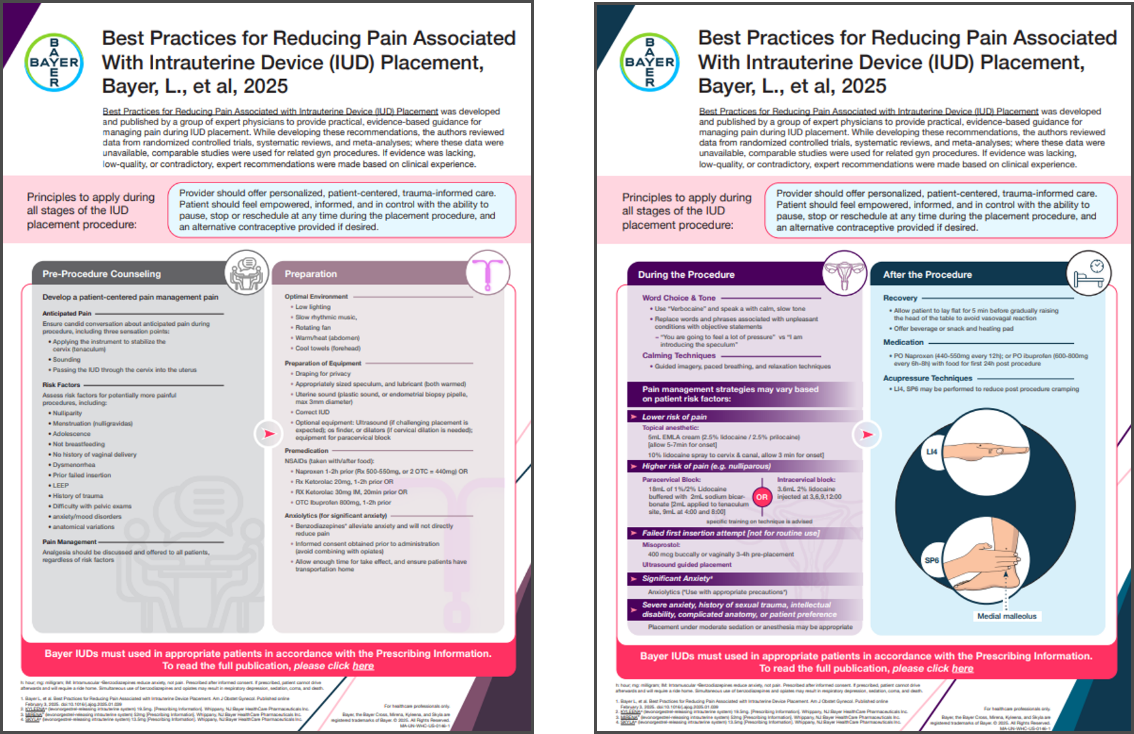
Best practices for reducing pain associated with intrauterine device placement, a recently published article (February 2025) by Bayer L, et al., provides a compilation of practical, evidence-based, expert-informed guidelines for the management of pain during IUD placement.
Access an infographic or interactive summary of the recommendations from “Best practices for reducing pain associated with intrauterine device placement,” by clicking below.
Reference:
Bayer L, et al. Am J Obstet Gynecol. 2025;232(5):409-421. doi: 10.1016/j.ajog.2025.01.039.
Pain Management for In-Office Uterine and Cervical Procedures, is a recently published article (July 2025) by the American College of Obstetricians and Gynecologists’(ACOG) Committee on Clinical Consensus–Gynecology. The purpose of this document was to provide evidence-based pain management offerings after a thorough review of all readily available publications and data on the subject.
Access the publication for “Pain Management for In-Office Uterine and Cervical Procedures,” by clicking below.
Reference:
Pain management for in-office uterine and cervical procedures: ACOG Clinical Consensus No. 9. Obstet Gynecol. 2025;146(1):161-177. doi: 10.1097/AOG.0000000000005911.